Your COVID-19 questions answered!

Sinai Health infectious disease expert Dr. Andrew Morris answers your questions about the new COVID-19 variant, how Sinai Health is responding, and whether you should get the vaccine.
1. What do I need to know about COVID-19, to protect myself from the new variant?
The new variant shouldn’t really change our approach at all. It’s still urgent we get this under control. The basics haven’t changed. We know that close contact, especially indoors, especially unmasked, and especially for more than a few minutes, really increases transmission. If we can figure out a way to minimize that for all people, it will go a long way to control the virus. The new variant is more transmissible. It seems the new variant may get us sick with fewer virus particles. But the fundamental means of transmission is the same. It’s not complicated, but it’s difficult, especially for some people. You really should avoid going into any buildings other than your home. If you are seeing other people, it should be over video, or outdoors, at a distance and masked. We know that sometimes people do need to go into a building other than their home. But we really need to work hard to minimize it. Only do it when absolutely necessary, minimize the time and take all precautions such as masking and physical distancing.
2. How is Sinai Health continuing to manage risk and deliver care after more than a year of responding to COVID-19?
The obvious difference that people would recognize right now is that our hospital in some ways is a much quieter place. Many physicians are providing care virtually. So that’s been the major shift. We’re doing everything possible to support people without them coming inside the hospital. We’re continuing to ramp that up and do everything possible to provide virtual care when appropriate.
On the other hand, we’re providing the necessary in-person care when people need it. The Emergency department is undergoing an expansion through this time. We’re expanding our ICU so we have more beds available for care. We’re figuring out ways to support our inpatients in a really safe way. For example, for people who need oxygen but don’t need to be on a ventilator, we’re finding ways to do this in the best way possible.
We’ve also taken a lot of measures to make sure everyone is staying safe. We’re screening very carefully whenever people come in. All of us are gowning, gloving, and masking for all new patients, not just to protect us but to protect our patients.
Like all hospitals, we’re guided by Ministry requirements around visitors. It’s been a challenging tightrope to walk and we’re trying to strike a balance between compassionate, patient-centred care while also making sure the hospital is safe for us all.
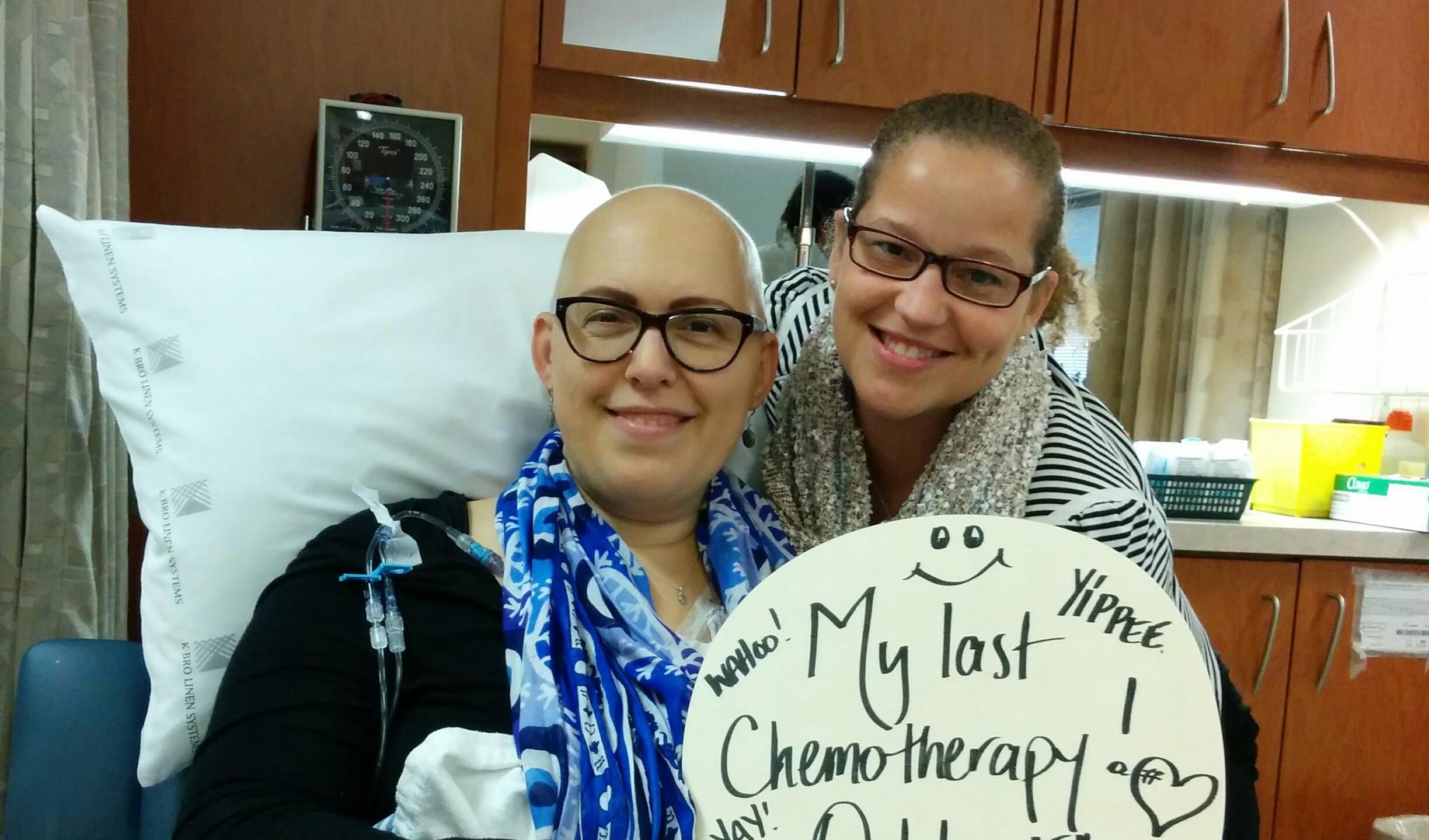
3. Should I be getting a vaccine if I have allergies or autoimmune disease? Is one dose enough?
There are very few reasons or indications not to get the vaccine. If you have had an organ transplant, are pregnant or breastfeeding, or have cancer, you can still probably get the vaccine, but its best to check with your healthcare provider to have a proper discussion. People like this will have worse outcomes if they do get COVID. If you’re worried, certainly discuss it with your doctor. People with allergies can get the vaccine, unless you have an allergy to polyethylene glycol or other vaccine components, in which case you should discuss it with your healthcare provider. In my mind there are very few reasons why someone should not get the vaccine.
Everyone agrees you need a second dose. The debate is how much time can pass before you have to get the second dose. It’s best to get the second dose on schedule but our supply chain has created obvious challenges. There is no Canadian jurisdiction that is considering only delivering one dose.